By Dian Ginsberg, MD, Board-Certified in OBGYN, Anti-Aging & Regenerative Medicine and Dawn Clark, Futures Architect, AI Systems Designer, Narrative Strategist
A collaboration between clinical expertise and human-centered innovation — redefining the future of women’s health.
Quick Summary
Midlife weight gain isn’t just about hormones — it’s about how multiple systems shift at once. Gut health, sleep, stress, metabolism, and even DNA all play a role. This article explains why old strategies stop working, what’s really happening inside your body, and the steps you can take to reset your biology.
The Bigger Picture
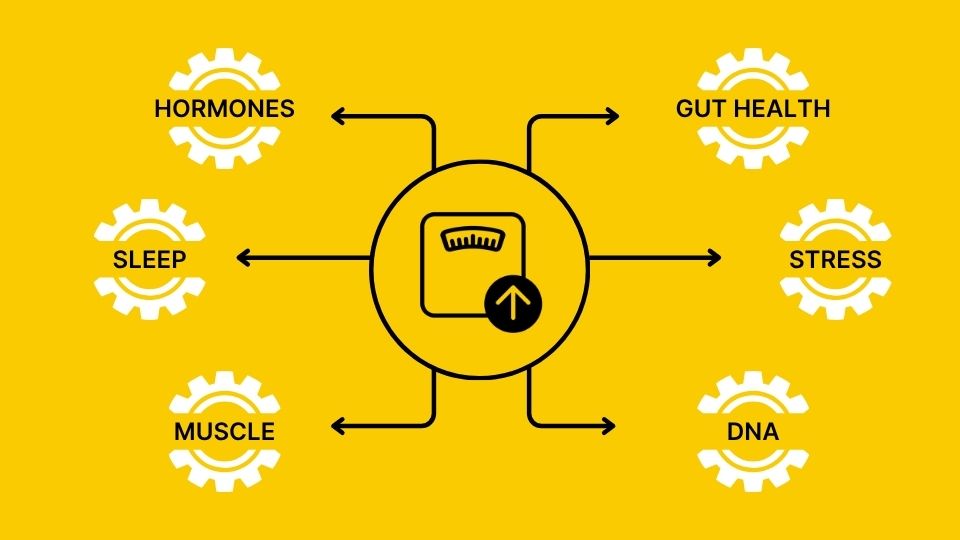
Midlife weight gain isn’t about one broken part — it’s about how all your systems work together. This is where precision medicine offers a deeper view — helping connect the dots between hormones, metabolism, gut, and DNA so your care reflects the whole picture.
Your body is like a high-performance engine, and your metabolism is the way that engine runs. Hormones, gut, sleep, stress, DNA, food, and muscle are the moving parts. When they’re tuned and fueled properly, your body runs smoothly. But when even one slips, the engine sputters — and weight feels stuck.
You’ve done what used to work: cut back on sugar, added spin classes, even tried intermittent fasting. But the weight won’t budge — especially around your middle. It feels like your metabolism is fighting back.

You’re not alone. Millions of women in midlife share this exact frustration. And too often, the only explanation they hear is: “It’s your hormones.”
Yes, hormones matter — but they’re just one part of a much larger system.
Just as puberty reshaped your body in your teens, midlife is another profound transition — not decline, but renewal. With the right tools, this stage can become your most powerful chapter yet.
The Myth: Hormones Alone Are to Blame
Estrogen, progesterone, and testosterone all change in midlife, influencing fat storage, muscle mass, and metabolism.
But they don’t act in isolation. Hormones interact with your gut, brain, and stress system — meaning weight gain isn’t just about estrogen “going down.” It’s about the ripple effects that follow.
The Reality: Interconnected Systems
You can think of your body like an engine powered by interconnected gears. There are many, but six of the biggest drivers of midlife weight gain are:
⚙️ Hormones — the shifting signals
⚙️ Gut — your inner ecosystem
⚙️ Sleep — the reset button
⚙️ Stress — the cortisol factor
⚙️ Muscle — the horsepower
⚙️ DNA — the silent amplifier
When these gears are aligned, your metabolism hums and your body converts food into energy efficiently. But when even one slips, the others strain — and the output of the engine (your metabolism) slows down. That’s when stubborn midlife weight shows up, especially around the belly.
Hormones — The Shifting Signals
Estrogen, progesterone, and testosterone shifts are real — they change where fat is stored, disrupt sleep, and reduce muscle mass.
But hormones don’t explain everything. They connect with every other gear in the system:
-
Low progesterone fragments sleep
-
Falling estrogen alters gut balance
-
Testosterone decline weakens muscle, slowing metabolism
Science Nugget
Declining estrogen, progesterone, and testosterone alter how the body uses and stores energy — explaining why fat often redistributes in midlife. (Kravitz et al., Obstetrics and Gynecology Clinics of North America, 2018)

Gut — Your Inner Ecosystem
Around age 35, gut bacteria begin to shift. Helpful species decline, while inflammatory strains thrive. This can drive:
- More cravings
- Slower nutrient absorption
- Low-grade inflammation
An imbalanced gut doesn’t just cause cravings — it slows your metabolism’s engine, making belly fat the hardest to budge.
Science Nugget
Lower gut diversity often coincides with higher insulin resistance in midlife women — especially around the abdomen. (Peters et al., International Journal of Women’s Health, 2022).
Michelle's Story
Michelle was 52, a woman who did everything “right.” She lifted weights, stayed consistent with cardio, and ate clean. Still, stubborn belly fat clung on, her cravings lingered, and her energy was slipping away.
Testing uncovered the hidden pieces: her estrogen and progesterone were low, disrupting sleep and metabolism, while her gut bacteria were out of balance and early insulin resistance was setting in.
Once those gears were tuned — with hormone support and a nutrition plan built around protein, fiber, and the right carbs — her body finally began to shift. Fat stores gave way, lean muscle returned, and her energy lifted. For the first time in years, Michelle felt like her body was hers again.

Sleep - The Reset Button
Falling progesterone fragments rest, while hot flashes and stress make nights worse. The hormonal effects are immediate:
- Ghrelin (the hunger hormone) → spikes, driving stronger cravings — especially for sugar and carbs.
- Leptin (the satiety hormone) → drops, so you don’t feel full even after eating.
- Cortisol (the stress hormone) → rises, pushing the body to store fat around the belly.
Low progesterone is a key factor here. As levels drop, deep sleep becomes lighter and more fragmented — raising cortisol and worsening midlife brain fog. Restoring balance often means more than sleep hygiene; it means addressing the hormonal and metabolic systems that control circadian rhythm.
Science Nugget
Sleep is now non-negotiable. Short sleep and high cortisol create a hormonal setup for weight gain in perimenopausal women (Kravitz et al., Obstetrics and Gynecology Clinics of North America, 2018).
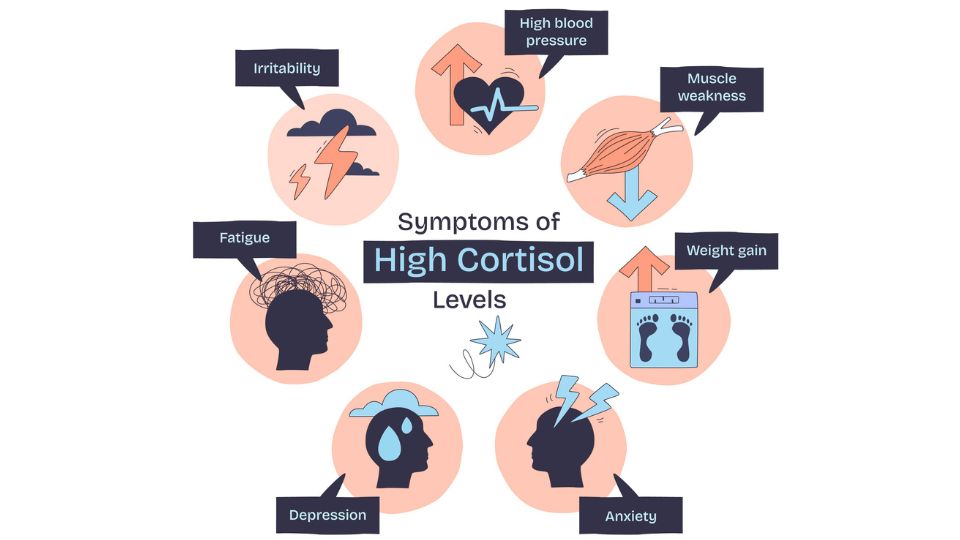
Stress — The Cortisol Factor
Cortisol naturally rises under pressure — and midlife is often peak pressure. But when stress becomes chronic, cortisol stays elevated.
This keeps the body’s engine revving high and drains the system:
-
Belly fat storage increases
-
Cravings for sugar and quick fuel spike
-
Insulin stays elevated
Science Nugget
Women with central (abdominal) fat show greater cortisol responses to stress — linking chronic stress to belly fat storage (Epel et al., Psychosomatic Medicine, 2000).

Muscle — The Horsepower
Muscle is your engine’s horsepower. In midlife, muscle mass naturally declines, lowering the “burn rate” of your metabolism. With less muscle, your body:
- Burns fewer calories at rest
- Becomes less sensitive to insulin — so sugar is more likely to be stored as fat
- Loses the strength and stamina needed for steady energy and recovery
That’s why weight-bearing exercise and strength training are more important than ever in midlife. Without enough muscle, your metabolism sputters and stubborn belly fat takes its place. But with regular resistance training and adequate protein, you preserve horsepower, improve insulin sensitivity, and keep your engine running strong.
Science Nugget
Hormonal decline in midlife reduces lean muscle mass, slows metabolism, and impairs glucose regulation — key drivers of fat gain. (Kravitz et al., Obstetrics and Gynecology Clinics of North America, 2018)

DNA — The Silent Amplifier
Some genes run quietly in the background early in life — but by midlife, stress, hormone shifts, and poor sleep can flip the switch and make them louder.
- FTO → linked to how your body stores fat. When activated, it makes belly fat gain more likely.
- MC4R → linked to appetite control. Variants can make hunger signals louder and fullness signals weaker.
- Other variants → can affect inflammation, how you process carbs, and how well you clear estrogen.
The takeaway:
Your DNA isn’t destiny — but under midlife pressure, it can amplify every other gear in your metabolism engine. Variants in genes like FTO and MC4R can affect how your body stores fat, regulates appetite, and even clears estrogen.Understanding your genetic blueprint reveals how your body processes hormones, nutrients, and stress — insights that explain why two women with the same labs can feel so different.
When this information is combined with hormone and metabolic testing, it provides a fuller picture — helping identify where your system needs the most support and how to work with your biology rather than against it. That’s how you unlock fat loss that once felt out of reach.
Science Nugget
Genetic testing can uncover tendencies toward carb sensitivity, appetite regulation issues, and inflammation. (Loos, R. J. F., et al., Nat Rev Genet, 2022) .
Lisa's Story
Lisa, 42, had tried everything — fasting, daily workouts, and countless diets. Still, the stubborn belly fat stayed put.
Testing revealed low progesterone, which was disrupting her sleep and leaving her estrogen dominant — a setup for both cravings and weight gain. DNA analysis uncovered a genetic variant tied to obesity risk and poor estrogen clearance.
Armed with this data, we built a personalized plan: targeted supplements to support estrogen detox pathways and optimize metabolism, plus a DNA-informed diet and exercise program that emphasized protein, fiber, and the right carbs.
As her hormones came back into balance and her metabolism reset, her belly fat finally began to let go. Her clothes fit again, her energy lifted, and she felt like she finally had her body — and her confidence — back under her control.

⚠️ The Trap of Quick-Fixes
When stubborn weight piles on in midlife, it’s tempting to grab at the next solution — a diet promoted by fitness models, a pill that promises effort-free results, or a social media “before-and-after” story that seems too good to be true. But quick fixes rarely deliver. In fact, they often pull women further from real answers.
Why they fall short:
- They ignore biology. Fad diets don’t account for midlife realities — hormone shifts, gut changes, muscle decline, or insulin resistance.
- They sell extremes and false shortcuts. From cutting entire food groups to swapping real meals for shakes, pills, or suppressants, these gimmicks focus on restriction instead of repair. But unless you address the gears driving your metabolism, stubborn weight will always return.
- They feed false hope. Slick marketing and dramatic testimonials push you to buy in — but when the promised results don’t show up, you’re left disappointed, doubting yourself, and feeling like the failure instead of the plan.
- They exploit influence. Celebrity and influencer promotions can be powerful — but they can also be misleading. Most are paid endorsements, designed to sell, not to reflect real science.
Why this matters:
Midlife weight gain isn’t a willpower problem — it’s a systems problem. Every month spent chasing gimmicks is a month the deeper imbalances remain unresolved.

Real Solutions: Getting Your Gears Back in Sync
Real, lasting change comes from understanding and working with your biology.
For some women, that starts with hormone profiling. For others, it may include gut or metabolic testing — and in certain cases, DNA insights or micronutrient evaluations that add another layer of clarity.
Even something as simple as correcting nutrient gaps can ease fatigue, quiet cravings, and lift brain fog.
The right mix depends on your unique blueprint. Ideally, this process is guided by a board-certified, experienced provider who can connect the dots across your systems, rather than offering one-size-fits-all fixes.
A Precision Medicine approach brings those systems into one clear picture — linking hormones, thyroid, gut, stress, and DNA — so care reflects the way your body truly works.
Ozempic® and Midlife Weight: What You Need to Know
GLP-1 medications like Ozempic® and Wegovy® are heavily promoted right now. But for midlife women, they come with serious trade-offs:
They don’t fix the root causes. GLP-1s don’t address hormone shifts, gut changes, muscle decline, or sleep disruption — the true drivers of midlife weight gain.
Muscle loss is a major concern. A significant share of weight lost is lean tissue. Losing muscle lowers metabolism and accelerates aging — the opposite of long-term health and vitality.
Other side effects are real. Digestive distress, nutrient gaps, and rebound weight gain after stopping are common.
No long-term strategy. Without rebuilding the underlying systems, weight often comes back — sometimes faster.
Why this matters:
If your goal is healthy longevity — living strong, with energy, muscle, and resilience — GLP-1s don’t provide that path. The better solution is strengthening your body’s core systems: hormones, gut, muscle, sleep, and stress. That’s how you achieve not just weight change, but lasting vitality.
That’s why our focus is different. Instead of chasing shortcuts that strip muscle and weaken resilience, we help women strengthen the very systems that drive long-term health.
Because midlife weight gain isn’t just about a number on the scale — it’s about energy, strength, and longevity. And when your gears are back in sync, you don’t just lose stubborn fat — you gain the power to live this chapter stronger than ever.

What You Can Do: Strategies That Work
-
Balance your gut
Eat 25–30 g of fiber daily, emphasize colorful plants, and consider targeted probiotics. A comprehensive stool test (e.g., GI-MAP) can uncover bacterial overgrowth, yeast, parasites, and digestive imbalances.
-
Lower carbs strategically
Prioritize whole, unprocessed carbs and limit refined ones. Glucose testing can reveal how your body processes carbohydrates as you age. DNA testing can also help determine carb sensitivity.
-
Lift weights (and add smart cardio)
Strength training 2–3x weekly preserves muscle and boosts insulin sensitivity. Add moderate cardio for cardiovascular health and stress reduction.
-
Prioritize sleep
Treat sleep as medicine. Stick to a routine, keep your bedroom dark and cool, and avoid screens before bed. If you’re in perimenopause or menopause, it may be time to check your progesterone levels — since low progesterone is a common, overlooked driver of disrupted sleep.
-
Manage cortisol
Walking outdoors, breathwork, and meditation all reduce fat-promoting stress hormones.
-
Check your hormones
If lifestyle changes alone stall, bioidentical hormone therapy may help recalibrate your system. But not every provider looks deeply enough. The right clinician will use in-depth testing that shows how your body metabolizes and absorbs hormones — while also considering gut health, glucose, stress, and even genetics.
You’re Not Broken — Your Gears Just Need Tuning
Midlife weight gain isn’t a failure of willpower. It’s what happens when the gears of your biology — hormones, gut, sleep, stress, muscle, and even DNA — fall out of sync.
When those gears grind against each other, your metabolism slows and fat feels stuck. But when you realign them, the entire system powers back up: cravings ease, energy returns, and weight begins to shift in a way that lasts.
This stage of life is not decline. Just as puberty reshaped your body into adulthood, midlife is reshaping you again — this time with wisdom, perspective, and the chance to invest in your long-term vitality.
With a Precision Medicine approach, every woman’s blueprint is honored. Your care is tailored to your unique biology, so the right gears get the right support. That’s how lasting change happens — from the inside out.
When you tune your biology, you don’t just lose stubborn belly fat. You gain clarity, strength, and the energy to design the next chapter on your own terms.
Midlife can be your strongest, most empowered chapter yet.
Ready to Feel Like Yourself Again?
You don’t have to do this alone. If weight feels stuck, energy is low, or your body isn’t responding the way it used to, the fastest way to get clarity is to start with the right first visit.
Use our Symptom-Guided Booking Page to choose your main concern and see the best first visit to book. We’ll guide you from there based on your results and goals.
About the Authors
Dr. Dian Ginsberg, MD
Dr. Ginsberg brings decades of clinical experience in women’s hormonal health to her practice. Certified in Anti-Aging & Regenerative Medicine, she is a nationally recognized expert in bio-identical hormone therapy and a leading voice in precision midlife care. In collaboration with Dawn Clark, she integrates deep clinical insight into an evolving model of women’s health that blends data, empathy, and innovation.
Dawn Clark
Dawn Clark designs intelligent, human-centered systems that transform how care is delivered and experienced. As the architect behind Precision FemCare’s digital innovation framework, she created the connective architecture linking science, story, and technology — reimagining how women access insight, empathy, and support between appointments. Her work brings depth, design, and emotional intelligence to the future of personalized healthcare.
Resources
- Beydoun, M. A., et al. (2013). Sex differences in the association of the apolipoprotein E ε4 allele with incidence of dementia and Alzheimer’s disease: A systematic review and meta-analysis. Dementia and Geriatric Cognitive Disorders, 35(1–2), 51–84. doi:10.1159/000345084
- Cattaneo, A., et al. (2017). The human gut microbiome as a key player in health and disease: A systems biology perspective. Clinical Pharmacology & Therapeutics, 102(1), 74–81. doi:10.1056/NEJMcibr1704542
- Loos, R. J. F., & Yeo, G. S. H. (2022). The genetics of obesity: From discovery to biology. Nature Reviews Genetics, 23(2), 120–133. doi:10.1038/s41576-021-00414-z
- Mahmoudi, E., et al. (2017). Genomics, epigenetics, and the “missing heritability” of complex diseases. International Journal of Molecular Sciences, 18(12), 2734. doi:10.3390/ijms18122734
- Peschken, C. A., & Esdaile, J. M. (2004). Systemic lupus erythematosus in North American Indians: A population based study. Journal of Rheumatology, 31(2), 325–332.
- Ussar, S., et al. (2016). Interactions between gut microbiota, host genetics, and diet modulate the predisposition to obesity and metabolic syndrome. Proceedings of the National Academy of Sciences of the United States of America, 113(51), E7101–E7108. doi:10.1073/pnas.1522933113
- Zhou, L., et al. (2022). Menopause, microbiome, and metabolic syndrome: Current insights. International Journal of Women’s Health, 14, 451–464. doi:10.2147/IJWH.S340491




