By Dian Ginsberg, MD, Board-Certified in OBGYN, Anti-Aging & Regenerative Medicine
and Dawn Clark, Futures Architect, AI Systems Designer, Narrative Strategist
A collaboration between clinical expertise and human-centered innovation — redefining the future of women’s health.
Quick Summary
Brain fog in midlife isn’t just “stress” or “getting older.” It happens when key systems — hormones, sleep, stress, gut health, nutrients, even genetics — shift out of sync. The result? Focus feels fuzzy and memory slips. The good news: once you understand what’s driving it, you can reset those systems and bring your clarity, confidence, and energy back online.
Introduction
You used to keep it all straight — deadlines, names, conversations. Now it’s like life is in soft focus. Words slip, focus scatters, and the harder you push, the fuzzier it gets.
This is brain fog — one of midlife’s most frustrating, least talked about shifts. Too often, women are told it’s “just stress” or “getting older.” The truth is far more complex — and far more hopeful.
Brain fog isn’t caused by one thing. It’s the result of interconnected circuits — hormones, gut health, sleep, stress, micronutrients, even DNA. When one shorts out, the others struggle, leading to fatigue, forgetfulness, and self-doubt.
The good news? Reset one system, and you can spark a cascade of clarity, energy, and confidence.
What Brain Fog Feels Like
Brain fog isn’t just a vague annoyance — it has a real impact on daily life. Women often describe it in their own words:
“My brain feels like it’s in slow motion.”
“I can’t concentrate or stay focused.”
“I keep forgetting simple things.”
“I lose my train of thought mid-sentence.”
“I can’t find the right words.”
The overall effect is more than just “a fuzzy day.” It feels like your sharpness is dimming — that you’re not firing on all cylinders.
The good news: brain fog isn’t permanent. It’s your body’s signal that systems are out of sync — and when you address the drivers, clarity, memory, and focus can all come back online.
6 Key Drivers of Midlife Brain Fog
Brain fog isn’t about one thing “breaking.” It’s what happens when your body’s key systems fall out of sync. Think of your brain as a network of circuits: hormones, sleep, stress, gut health, nutrients, and even DNA.
When those circuits are in balance, signals fire smoothly and clarity flows. But when even one falters, the others strain — and focus clouds over.
The hopeful part? Each of these systems can be brought back into balance. Here are the six key drivers of midlife brain fog — and why resetting them can restore your sharpness.
Ready to Clear Your Brain Fog?

Estrogen & Glucose: The Sharpness Factor
Estrogen does far more than regulate reproduction — it’s a performance hormone for the brain. It fuels acetylcholine, the neurotransmitter behind memory, word recall, and processing speed. When estrogen dips or swings in midlife, circuits falter — and everyday life shows it:
- Names and words slip just out of reach.
- Focus scatters, and multitasking feels harder.
- Afternoon crashes and cravings set in, leaving you foggy after meals.
These shifts often overlap with blood sugar instability. Without estrogen’s steadying effect, glucose isn’t handled as efficiently — fueling fatigue, irritability, and mental cloudiness.
Why it matters: Advanced hormone profiling (beyond a single blood test) reveals how your body metabolizes and clears estrogen. For many women, carefully tailored bioidentical therapy helps restabilize these pathways — restoring clarity, steady energy, and mental acuity.
Science Nugget
Estrogen directly supports acetylcholine — the neurotransmitter that powers memory and focus. Declining estrogen is linked to slower processing speed and more memory lapses in midlife women. (Russell et al., Neurotherapeutics, 2019)

Progesterone, Sleep & Cortisol: The Calm-Reset Loop
Progesterone, Sleep & Cortisol: The Calm-Reset Loop
Progesterone is the body’s natural “calm and sleep” support — and it often starts declining earlier than most women realize, sometimes in the mid-30s. As levels fall, you lose a built-in stress buffer and a key aid for deep, restorative sleep. Add midlife stress, and cortisol rises — keeping the brain on alert when it should power down.
What this looks like day to day:
- Lighter, restless sleep — harder to fall or stay asleep; more night waking
- Tired-but-wired nights — a racing mind at bedtime or 3 a.m.
- Shorter fuse by day — irritability and reactivity spike
- Memory misfires — poor sleep plus high cortisol blunts recall and focus
These patterns reinforce each other: fragmented sleep elevates cortisol, and elevated cortisol further fragments sleep — tightening the fog.
Why it matters: Because progesterone decline often begins earlier than expected, supporting it (when appropriate), restoring deep sleep, and smoothing the daily cortisol curve can quickly lift brain fog. Options include micronized time-release progesterone, cortisol-curve testing, and tailored evening routines that help your brain downshift into true recovery.
Science Nugget
Studies show that declining progesterone during the menopause transition is significantly associated with poorer sleep quality, reduced efficiency, and greater sleep fragmentation — outcomes closely tied to next-day cognitive performance and memory. (Menopause, 2024)
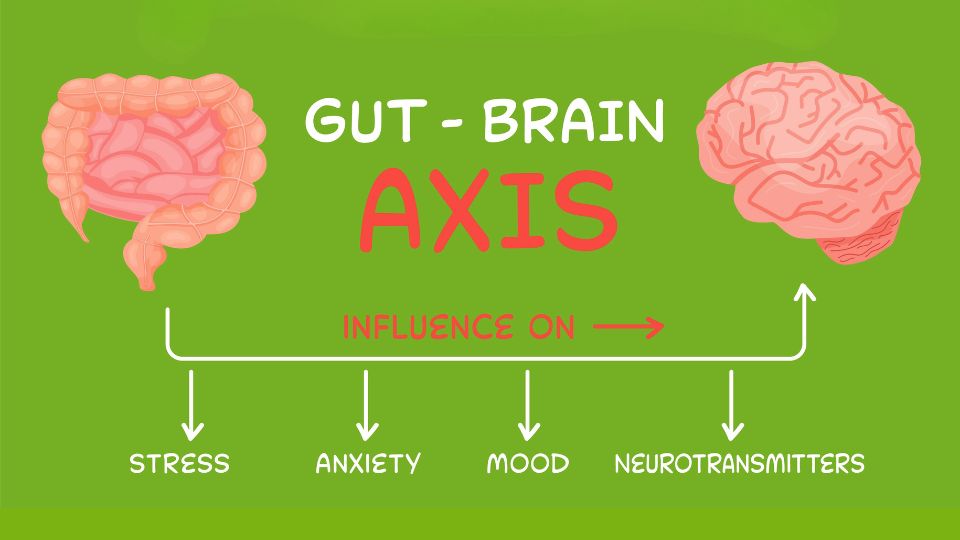
Gut–Brain Axis: Mood, Focus & Microbes
Your gut doesn’t just digest food — it helps power your brain. Nearly 90% of serotonin (for calm and mood) and much of dopamine (for motivation and focus) are produced in the gut. When gut microbes are balanced, they support sharp thinking and emotional steadiness.
But in midlife, that balance often shifts:
- Helpful strains decline while inflammatory ones grow.
- Neurotransmitter production falters, clouding mood and focus.
- Sugar cravings spike, fueling fatigue and fog.
Why it matters: Resetting your gut often means resetting your mind. Personalized nutrition , probiotics, and fiber-rich foods can restore microbial balance, while advanced testing helps pinpoint what’s really out of sync. When this axis is back online, many women notice their clarity, energy, and mood all improve.
Science Nugget
Nearly 90% of the body’s serotonin — essential for mood and focus — is produced in the gut. Disruptions in the microbiome can directly impair serotonin and dopamine signaling, leaving you foggy and fatigued. Frontiers in Microbiology, 2018

The Emotional Loop: Anxiety Feeding the Fog
Brain fog doesn’t just cloud memory — it stirs up emotions that deepen the fog. Many women describe the sinking fear of forgetting a word in a meeting, rereading the same page again and again, or blanking mid-thought. These moments can feel like evidence that something is “wrong,” and the fear itself becomes part of the problem.
- The trigger: Small slips in recall or focus spark worry and self-doubt.
- The loop: Stress activates the limbic system — the brain’s emotional center — and reduces access to the prefrontal cortex, which is responsible for logic, attention, and higher reasoning.
- The spiral: The more you notice the slips, the more anxious you feel. Anxiety raises cortisol, disrupts sleep, and creates a self-reinforcing cycle of fog and fear.
Why it matters: Recognizing this loop is freeing. Brain fog in midlife isn’t “just in your head” — it’s a biological-emotional cycle that can be interrupted. Calming cortisol, restoring sleep, and layering in self-compassion (instead of self-criticism) help break the loop. As the biology resets, confidence and clarity return.
Science Nugget
Neuroimaging shows that stress and hormonal decline heighten limbic activity while reducing prefrontal cortex efficiency — linking anxiety directly to impaired memory and focus. (Mosconi et al., Scientific Reports, 2021)

DNA: The Hidden Blueprint
Why do some women only experience mild brain fog, while others feel like their sharpness disappears almost overnight? Genetics often provide the answer . Certain variants influence how efficiently your body clears estrogen, how dopamine and other neurotransmitters are processed, and how resilient your stress response is. When these variants interact with midlife hormone shifts, the fog can feel heavier and harder to shake.
- Estrogen metabolism genes: Slower clearance can lead to estrogen dominance, anxiety, and foggier thinking.
- COMT variants: Affect dopamine breakdown, leaving some women more prone to fatigue, low motivation, or “mental crash.”
- Stress response genes: Can magnify the effects of cortisol, making stress feel more mentally draining.
Why it matters: DNA isn’t destiny. But it does reveal where your vulnerabilities — and your opportunities — lie. With testing, providers can design precise strategies: tailoring diet, supplements, stress relief, and hormone support to your unique blueprint. Instead of trial and error, you get a clear, personalized path toward lifting the fog and restoring mental sharpness.
Science Nugget
Genetic variants linked to estrogen metabolism and dopamine pathways are associated with differences in cognitive performance during midlife. (Dumas et al., Neurobiology of Aging, 2018)
Micronutrients: The Missing Links
Micronutrients: The Missing Links
Even when hormones, gut health, sleep, and stress are addressed, your brain still needs raw materials to function at its best. In midlife, absorption often shifts and deficiencies become more common — quietly clouding thinking, draining energy, and worsening brain fog.
- B vitamins (B12 & folate): Fuel neurotransmitter production and protect memory.
- Magnesium: Calms the nervous system and supports deeper, restorative sleep.
- Omega-3s: Reduce inflammation and keep brain cell membranes flexible for sharper signaling.
- Vitamin D: Supports mood, cognition, and immune balance — often low in midlife women.
- CoQ10: Fuels mitochondria, your brain’s energy factories, and protects against oxidative stress.
Why it matters: Micronutrient gaps may not cause brain fog on their own, but they often magnify it — like running a high-performance engine on low-grade fuel. The good news is that these gaps are among the easiest to identify and correct, giving your brain the steady support it needs to stay sharp.
Science Nugget
Research links deficiencies in B vitamins, magnesium, and vitamin D with impaired cognitive performance in midlife women.
(Erdélyi et al., Nutrients, 2023)
Resetting Your Circuits: How to Clear the Fog
Brain fog isn’t permanent — it’s your body’s signal that key systems need attention. When you reset even one circuit, the others often begin to realign. Here are proven strategies to restore clarity:
- Check your hormones
Advanced hormone profiling (not just a single blood draw) shows how your body metabolizes and clears estrogen and progesterone. For many women, bioidentical therapy provides the foundation for restored clarity and sharper cognition. - Prioritize sleep & manage cortisol
Evening routines, calming practices, and cortisol curve testing help reset your natural rhythm. Deep, restorative sleep is often the fastest way to lift brain fog. - Rebuild your gut
A stool test (e.g., GI-MAP) can uncover imbalances, inflammation, or hidden microbes that disrupt brain chemistry. Personalized nutrition, probiotics, and fiber-rich foods restore the gut–brain connection. - Correct nutrient gaps
Even subtle deficiencies cloud thinking. B vitamins, magnesium, vitamin D, omega-3s, and CoQ10 are among the most common missing links in midlife. Testing pinpoints where support is needed, and replenishment often lifts fatigue and steadies memory.
- Interrupt the emotional-anxiety loop
Self-compassion strategies, mindfulness, and stress resilience tools break the anxiety–fog cycle. Calming cortisol and reframing self-doubt help confidence — and clarity — return. - Move your body
Cardio boosts oxygen delivery to the brain, while strength training stabilizes glucose and neurotransmitters. Together, they’re powerful medicine for focus and memory.
The takeaway: Brain fog isn’t decline. With the right insights and support, midlife can become a chapter of renewed clarity, confidence, and creativity.
Carla’s Fog, and Her Way Out
Carla, 46, was a respected attorney known for her sharp focus. But lately, she struggled to recall names, lost her edge in conversations, and found herself rereading paragraphs to grasp what once came easily. “I was embarrassed,” she said. “What if people started to notice?”
The usual fixes didn’t help. Testing revealed the real drivers: low progesterone and estrogen dips were blurring her memory and focus, high evening cortisol was draining her concentration, and she was missing key micronutrients that fuel brain clarity.
With bioidentical hormone therapy, stress support, gut rebalancing, and targeted nutrients, her clarity returned. “I finally felt like myself again,” Carla said. “Not just keeping up — but confident and in control.”
Brain Fog Isn’t Forever: It’s Fixable
Brain fog isn’t decline, and it isn’t “just getting older.” It happens when key systems in your body — hormones, sleep, stress, gut health, nutrients, even DNA — fall out of sync.
These systems can be brought back into balance. When they are, clarity returns, memory steadies, and focus sharpens.
Midlife isn’t the end of your sharpness. It’s the start of a new chapter — one where the right insights and a personalized plan help you reclaim your energy, confidence, and mental edge.
Ready to Get Your Clarity Back?
You don’t have to push through or “just live with it.” At Precision FemCare, we uncover what’s driving your brain fog and create a plan to bring your sharpness back online. There are two simple ways to begin:
Start with Dr. Dian Ginsberg if you suspect hormones are at the core. She’s a nationally recognized expert who interprets your labs and tailors care to your biology.
Start with our certified nutritionist if you’d like to focus first on gut health, micronutrient testing, DNA-informed diet, and personalized nutrition with glucose tracking.
Either path reveals the root causes of brain fog and builds a roadmap toward steady focus, stronger energy, and renewed confidence.
About the Authors
Dr. Dian Ginsberg, MD
Dr. Ginsberg brings decades of clinical experience in women’s hormonal health to her practice. Certified in Anti-Aging & Regenerative Medicine, she is a nationally recognized expert in bio-identical hormone therapy and a leading voice in precision midlife care. In collaboration with Dawn Clark, she integrates deep clinical insight into an evolving model of women’s health that blends data, empathy, and innovation.
Dawn Clark
Dawn Clark designs intelligent, human-centered systems that transform how care is delivered and experienced. As the architect behind Precision FemCare’s digital innovation framework, she created the connective architecture linking science, story, and technology — reimagining how women access insight, empathy, and support between appointments. Her work brings depth, design, and emotional intelligence to the future of personalized healthcare.
References
- Chai, Y., et al. (2021). Epigenetic regulation of aging and age-related diseases: Mechanisms and interventions. Frontiers in Cell and Developmental Biology, 9, 686528.
- Conde, D. M., et al. (2021). Menopause and cognitive impairment: A narrative review of current knowledge. World Journal of Psychiatry, 11(8), 412–428.
- Dhana, K., et al. (2019). Obesity and the risk of dementia in U.S. women and men by race/ethnicity and age: A prospective cohort study. Obesity, 27(12), 1994–2002.
- Erdélyi, A., et al. (2023). The importance of nutrition in menopause and perimenopause—A review. Nutrients, 16(1), 27.
- Jansen, I. E., et al. (2019). Genome-wide meta-analysis identifies new loci and functional pathways influencing Alzheimer’s disease risk. Neurobiology of Aging, 66(1), 8.e1–8.e14.
- Menopause. (2024). Declining progesterone during the menopause transition and its association with sleep quality and cognitive performance. Menopause Journal.
- Ouanes, S., & Popp, J. (2019). High cortisol and the risk of dementia and Alzheimer’s disease: A review of the literature. Frontiers in Aging Neuroscience, 11, 43.
- Peters, B. A., et al. (2022). Spotlight on the gut microbiome in menopause. Frontiers in Aging Neuroscience, 14, 9379122.
- Russell, J. K., et al. (2019). The role of estrogen in brain and cognitive aging. Neurotherapeutics, 16(3), 649–665.
- Yano, J. M., et al. (2018). The Microbiota–Gut–Brain Axis: From Neurons to Behavior. Frontiers in Microbiology, 9, 1095.
- van den Egmond, L. A., et al. (2022). Body mass index, midlife weight change, and risk of dementia in women and men: A prospective cohort study. Obesity, 30(8), 1665–1673.




